Catheter Associated Urinary Tract Infection
A catheter-associated urinary tract infection (CAUTI) can happen when bacteria enter the urinary tract through a catheter, a thin tube inserted into the bladder to drain urine. This type of infection is common among people who require a catheter and is one of the most common healthcare-associated infections, but it is both preventable and treatable.
Catheters are used to support the bladder when people are unable to urinate naturally. This may be due to bladder weakness, spinal injury, or other nerve damage affecting the ability to pass urine. They may also be used following surgery to assist healing, or if bladder outflow is obstructed, such as an enlarged prostate, urethral strictures or renal/bladder stones.
Catheter UTI symptoms
Catheter-associated urinary tract infections typically have the following symptoms:
- Cloudy or foul-smelling urine
- Fever
- Chills
- Fatigue
- Discomfort in the bladder, lower back, or pelvic area.
- Pain in the urethra
- Blood in the urine
- Increased urgency and frequency to urinate
- Catheter leakage or unusual sediment in the urine
- Older people may appear confused or have behavioural changes
- Dark urine (though this may be because you need to drink more)
- Pain, burning, or stinging when passing urine
The symptoms are generally similar for men and women. As well as the above, men might have penile discomfort, while women might report vaginal irritation or pelvic pain.
If you suspect a catheter UTI, consult a doctor or nurse immediately.
Causes of catheter-associated urinary tract infections
Catheter-associated urinary tract infections represent a common and preventable complication of urinary catheterisation. Inserting a catheter runs the risk of introducing bacteria into the urinary tract, leading to infections in various areas such as the urethra, ureters, kidneys, or bladder. There will always be bacteria in the urine if a catheter has been in place for more than a few days.
This does not mean you have a urinary infection, but if you develop symptoms, antibiotics may be needed.
Certain individuals are at higher risk of developing CAUTIs:
- The amount of time a catheter stays in place is a significant risk factor
- Using an indwelling catheter for a long time increases the likelihood of bacterial colonisation, which can lead to infections.
- Alternatively, repeatedly handling or disconnecting the catheter can also increase the likelihood of introducing pathogens into the urinary tract.
- Poor insertion techniques and hygiene practices leave people susceptible to CAUTIs.
- Patients with diabetes, kidney disease, weakened immune systems, or those on immunosuppressive medications are particularly vulnerable to CAUTIs.
- The elderly are more vulnerable.
- Women are more susceptible to UTIs due to a shorter urinary tract.
- Those experiencing extended hospital stays and in long-term care settings
- Low mobility can contribute to a build-up of bladder sediment
- Poor hydration
CAUTIs in patients with spinal cord injuries
Patients with spinal cord injuries have a greater risk of CAUTIs. Their condition often requires prolonged catheterisation, which increases the likelihood of bacterial colonisation of the urinary tract.
Impaired bladder function and reduced mobility in patients with spinal cord injury contribute to urine stagnation and a buildup of sediment, which promotes bacterial growth. Reduced immune responses linked to long-term illness further complicate this issue.
Combatting CAUTIs in this group of patients requires integrating best practices such as routine catheter care, early removal when feasible and the use of antimicrobial-coated catheters.
Catheter-associated UTIs in the elderly
Older adults are also more likely to develop catheter-associated urinary tract infections. This is due to age-related physiological changes and comorbidities. These factors include weakened immune systems, reduced bladder elasticity and chronic medical conditions like diabetes or neurological disorders.
If left untreated, infections can escalate to severe complications such as urosepsis, renal damage, or systemic inflammatory response. Regular monitoring and replacing catheters as soon as signs of infection are spotted can reduce risks.
CAUTI prevention strategies
There are several ways in which CAUTIs can be prevented in both the home and healthcare environments.
Hand hygiene
Proper hand hygiene is crucial to preventing CAUTIs. Wash your hands with soap and water or use alcohol-based sanitisers before and after catheter insertion or handling. Clean the catheter daily with warm water and a mild, non-irritating soap. Move outward from the catheter insertion site to perform careful, unidirectional cleaning.
Daily catheter cleaning
Daily cleaning of the catheter and the insertion site lowers bacterial contamination. Wash your hands prior to cleaning and then use a mild soap and water to clean the insertion site and the tubing. Always wipe away from the body and take care not to pull on the tubing. Saline or antiseptic solutions can be used and harsh rubbing should be avoided to prevent tissue irritation.
Urine bag management
Proper urine bag management reduces the risk of infection by maintaining a closed drainage system. Drain bags before they’re two-thirds full and keep them below bladder level without touching the floor.
To minimise contamination, make sure the system is disconnected only when necessary. Ensure bags or catheter valves are changed on a weekly basis and bags are visibly clean on a daily basis.
You may shower with a catheter in situ, it is advisable to empty the bag first and remove and replace the fabric straps.
Catheter stabilisation
Catheter stabilisation prevents movement, reducing the risk of urethral trauma and infection. Anchor straps and leg bands can keep catheters in place.
Handling precautions
Avoid using unsterilised or ungloved hands when handling a catheter and replace the device immediately if this isn’t followed.
Hydration management
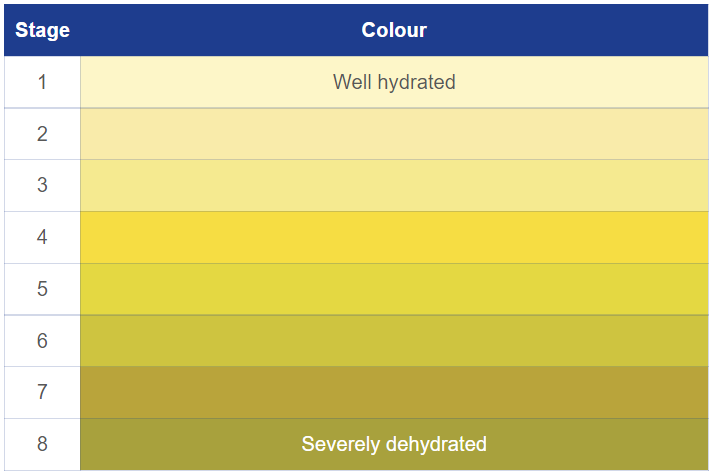
Drink 1.5 – 2.5 litres of fluid daily to stay fully hydrated; monitor urine colour as a hydration indicator.
Ensuring you drink enough water promotes consistent urinary flow, helps flush potential pathogens and reduces the risk of catheter obstruction.
CAUTI treatment
To treat CAUTIs effectively, the infection must be addressed while reducing the risk of recurrence.
Antibiotics
Antibiotics are commonly used to treat CAUTIs by targeting pathogens identified through urine culture tests. Broad-spectrum antibiotics, such as ciprofloxacin or trimethoprim-sulfamethoxazole, are often initially prescribed. Once the causative organism is identified, narrow-spectrum antibiotics like nitrofurantoin are used.
Prolonged use of antibiotics can lead to drug resistance. Short-term courses, usually lasting 5-7 days, are preferred unless complications arise, such as severe symptoms or underlying health issues. Intravenous antibiotics, like ceftriaxone, are given in severe or hospitalised cases.
If oral antibiotics are used, ensure the catheter is changed within 24-48 hours as it will be colonised. A urine sample can be taken from the new catheter if needed for cultures. If IV antibiotics are used, the catheter can be changed after the first dose.
Preventing recurrent infections
Preventing recurrent CAUTIs involves addressing catheter use and implementing hygiene practices. Prompt catheter removal reduces infection risks as soon as it’s no longer necessary. Intermittent catheterisation is recommended where possible.
Sterile techniques during catheter insertion and maintenance reduce the risk of contamination. Daily catheter care, which includes cleaning the meatus and ensuring proper urine flow, helps prevent infection buildup. Antimicrobial-coated or silver-alloy urinary catheters may offer additional protection for high-risk patients.
Hydration promotes urinary tract health by flushing out bacteria and sediment, so drink at least 1.5 – 2.5 litres of water daily. This is a guide; you may be advised to drink more or less than that depending on your medical or physical condition.
Your hydration level can be monitored by the colour of your urine; you should aim for a pale straw colour. Having an awareness of symptoms and treating the infection as early as possible minimises the risk.
