
It’s not uncommon to feel like you won’t be able to cope after ostomy surgery. Early on, there’s so many things you want answered. Being part of the online ostomy community answered a whole heap of questions I didn’t even know I had! Then there’s concerns about what you can and can’t do. Spoiler alert – the list of things you can’t do is actually very short.
I’ve previously written a post which includes a bunch of resources for common questions, such as emptying, showering, food, travel, and lots more!
I’ve shared my experiences before, having had an ileostomy on three different occasions myself. This time, I want to include some experiences from other ostomates too. I can’t pretend I hold all the answers, but I believe it is important that you know you’re not alone.
I asked the community, what did you struggle with the most after ostomy surgery?
The intestine is close to numerous internal organs and nerves, so it carries a lot of potential risks, many of which can severely impact quality of life for ostomates. Many of us feel these weren’t explained to us thoroughly enough before surgery. Some people even said they didn’t think they would have wanted surgery had they known.

Sexual and reproductive health
Women struggled with reproductive issues, some of which had been discussed pre-surgery, and some of which were a complete surprise. Infertility, painful sexual experiences, and premature menopause were all mentioned. An increase of heavy, or ‘pooling’ discharge is also fairly common, but rarely discussed. All of which can be very difficult to deal with, whether they were expected or not, and can impact self-confidence and quality of life.
Colorectal surgery in men carries risks if damage to certain nerves occur. This may cause erectile dysfunction and retrograde ejaculation (when semen enters the bladder). It has an understandably negative impact on quality of life, and again, self-confidence. Many men say they weren’t made aware of these risks prior to surgery, making it even more distressing for them.
Bladder complications
Interstitial cystitis, also known as bladder pain syndrome, is more common in inflammatory bowel disease, especially following ostomy surgery. Symptoms include pelvic pain, a frequent and urgent need to urinate, or difficulty passing urine. On the other end of the spectrum, an underactive bladder can also be a problem. Symptoms include hesitancy, sensation of incomplete emptying, straining, and recurrent infections.
Again, living with these symptoms can detrimentally impact quality of life, and can affect other areas such as sleep and lead to anxiety about, or avoidance of, activities and travel.
Hernia
Parastomal hernia is the most frequent complication associated with the creation of an ileostomy or colostomy. Not being made aware of the increased risk of hernia, or how to minimise those risks was a common complaint, with many ostomates not realising until it was too late.
If surgery to repair the hernia can be avoided, that’s usually the recommendation, as long as it’s not causing acute issues. Recurrence rates are now much lower due advancements in repair methods. The use of synthetic mesh has decreased the recurrence rate, which is now thought to range between 7 and 18%.
Rectal stump complications
If you’ve had your rectum or rectal stump left intact, it can be quite the shock to feel the urge to go to the toilet and pass some mucous or even blood into the bowl, if you weren’t made aware it was likely going to happen! It doesn’t realise it’s not performing its regular duties, so it creates the mucous to help the waste pass through. So, unfortunately, remaining rectum usually means passing mucous, for some it’s occasionally, and for others it’s very regular.
It’s even worse if it’s accompanied by urgency and frequency. In IBD in particular, the remainder can accommodate active disease, often requiring medications (sometimes administered rectally direct to the site) and possibly even requiring further surgery to remove it.
Crazy unpredictable output
The initial erratic output was also mentioned as a concern. This can be a factor in regular leaks in the initial period after surgery. It’s totally understandable, because if no-one tells you that this is not your normal from now on, it’s going to be a worry. It’s not uncommon to have really loose and frequent output following stoma surgery, which settles down gradually as you settle into a routine. Your intestine needs time to heal, and the inflammation takes time to subside.
You may be prescribed anti-diarrhoeal medications and have fluids administered via IV whilst in hospital. You may also be discharged with medications to slow output down, which you may be able to reduce over time, or continue to take long-term.
Dehydration risk is higher during this frequent loose stool period. According to a 2019 study, 29% of post-ileostomy discharges are readmitted, most commonly due to dehydration.
Dehydration
Hydration is a complicated topic. How much fluid you need will depend on a number of factors, such as the type of stoma you have, your current health, weight, the local climate, and how physically active you are. You might need to increase your daily salt intake, or drink oral rehydration solution, but you might also manage just fine without!
I have to take electrolytes daily, but I still find the summer months really difficult. There’s no concrete formula that tells me how much I should drink depending on the weather, or if I’ve been gardening for two hours… I’m good at recognising dehydration now, so I can at least act on it quickly. For me, dehydration often comes with passing a lot of liquid output. This is due to my electrolytes being off balance, and would be a “normal” person’ s diarrhoea.
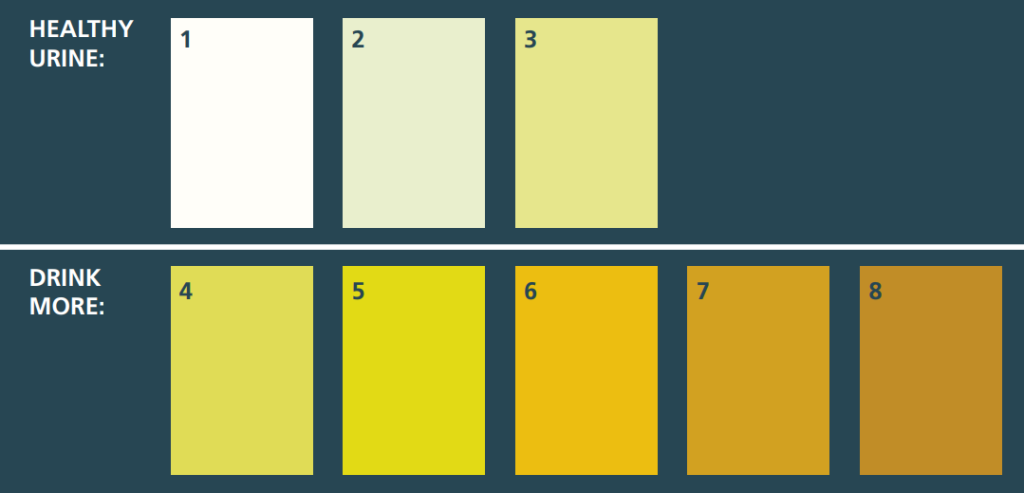
Know the symptoms; dry mouth, thirst, light-headedness or feeling dizzy, fatigue, headache, passing less urine which is dark or strong smelling, muscle cramps. If you’re not thirsty and you’re urinating frequently, and it’s colourless or light yellow, you’re probably good.
Leaks and sore skin
Many people were worried about leaks and felt they didn’t get enough support or advice for solving or avoiding them.
Advice on how often to change your bag seems to vary a lot too, often resulting in leaks for longer wear time advice and sore skin due to changing too often. In reality, we’re all different. We’re working around different lifestyles too, which do have to be taken into consideration when organising our routine.
It sounds like people often begin to panic in the early days after surgery, because they have a few leaks before everything settles down. They also seem to lack the reassurance that it’s not something that will happen regularly.
The amount of different bag manufacturers and supporting products, often designed to help prevent leaks, is incredible. Nobody should be dealing with frequent leaks!
Solo bag changes
There’s also fears about going it alone, with many ostomates feeling like they’re not properly prepared or ready for going home and doing bag changes all by themselves. I can definitely confirm that it’s scary and slow to start, but before you know it, the routine is taking less than a minute out of your day!
Emptying away from home
Ostomates reported being worried about emptying their bag away from home, often cutting outings short to go home and empty, or avoiding eating before going somewhere.
I think the main worry comes down to smell. I carry a “spray before you go” bottle everywhere with me, and they do a great job at masking odour, whether it’s public toilets or a friend’s house. There’s always the option to open a window too!
Body confidence and scars
Many people are upset about their new body, and the scars that are left behind.
Some people are able to embrace their stoma and their scars. For others, they are a constant reminder of a traumatic experience. I’ve talked about body confidence before, and how I grieved for my pre-stoma body. When I had my first stoma reversed, I had scars from the midline incision, drain, and ileostomy. They basically covered my abdomen, and constantly reminded me of two dreadful years, full of leaks, burnt skin, misery, and isolation. I hated them. So much so, that I had my stoma scar tattooed over. I wanted to forget the period in which I felt nothing but embarrassment, weakness, and shame.
For me, it was the online ostomy community that helped me reach acceptance. Now, I’m proud of my scars. I even regret covering the old ostomy one. It’s been quite the journey for me, and it’s definitely not one that can be rushed through.
Fittleworth’s “I’m still me” ostomates body confidence resource may be able to help you start that journey.
What to wear?!
Being a bit lost in the clothing department is totally relatable to me. It can feel super complicated trying to accommodate your new accessory. Not knowing whether to wear waistbands above or below. And of course, having to deal with psychological impact of what your body just went through, including self-confidence issues. I previously wrote about my experience, and shared tips and specialist clothing sites.

Confused by food
Poor dietary advice is a common complaint. We’re often given lists of safe foods and foods to avoid and sent on our merry way.
Many people aren’t told that this is only supposed to be for the initial healing period, and then new foods should be introduced slowly. This leaves many ostomates living on a restrictive diet, scared to try new foods. It’s prudent to use a food diary, and to try each new food a few times, a good few days apart, before writing it off if the first time didn’t go well. Your tolerances might also change slightly over time.
Fittleworth’s free Ostomates Kitchen recipe guide offers some great ideas for meals, as well as alternatives for foods you may not be able to tolerate.
Just needing someone to talk to
Most of us have experienced feeling a little lost and lonely. Mental health support after stoma formation is a necessity, in my opinion. Whether that comes from a professional, or just someone who understands what you’ve been through. Chatting to those with lived experience can be invaluable. It’s important to understand that your journey is uniquely yours, but at the same time, there are people out there who get it. Who have experienced similar things and have faced similar struggles. And then there’s those close to you, who may never fully get it, but who care enough about you to want to be involved in helping you feel better.
If you’d like to talk with other ostomates, check out the Fittleworth ostomate group. If you want to talk privately, my inbox is always open.
We hope you enjoyed this article from our guest blogger. They are expressing their views or knowledge on a topic because of their experience & background. Some of the opinions expressed may not reflect the views of Fittleworth or your NHS professional.
It goes without saying, but this is not clinical advice. Each person will have an individual set of medical factors to consider. So please do not to make significant changes to your diet, exercise or treatments before consulting with a NHS professional.
Sahara was admitted to hospital and diagnosed with Ulcerative Colitis at the age of 19,  after just two weeks of being incredibly unwell.
after just two weeks of being incredibly unwell.
One week later, she had emergency surgery to remove her colon and rectum, and had her first ileostomy. A turbulent journey followed; a multitude of treatments, complications, seven surgeries, a failed J-Pouch, and three ileostomies later, she is living with a permanent stoma and is a pro-active IBD and ostomy advocate.
Sahara joined the online IBD and ostomy community in 2014, and it very quickly became apparent to her that whilst awareness is important, even more important than that is providing support to others as they navigate the stormy waters of life with IBD, or an ostomy.
She runs #IBDSuperHeroes fundraising and awareness campaign, and the Facebook support group. She is a blogger for InflammatortyBowelDisease.net and an IBD Patient Consultant for merakoi – bridging the gap between patients and healthcare. She gets involved with research whenever she can, and is a volunteer for Cure Crohn’s Colitis, where she donates her time and expertise in social media marketing and content creation.
